Atrial fibrillation: Causes, symptoms and treatment
What is atrial fibrillation (AFib)? Is it dangerous? What are causes for the rapid and irregular heartbeat? Who needs blood thinners? Please find answers to these and other questions in the following text.
How common is atrial fibrillation?
Atrial fibrillation is the most common benign cardiac arrhythmia. It mainly affects older people. With increasing age, the risk of getting atrial fibrillation rises.
From the age of 70, up to 15 out of 100 people suffer from atrial fibrillation. Between the ages of 60 and 70 it affects 5% of the population and between 50 and 60 1%. Experts assume that the number of cases will continue to increase in the future, not because we are getting sicker, but because we are getting older.
Cardiovascular diseases such as coronary heart disease, high blood pressure and heart damage are one of the main causes of cardiac arrhythmias in older people including atrial fibrillation.
Causes
What exactly causes atrial fibrillation?
Atrial fibrillation is usually caused by a damage of the heart muscle due to heart disease. This damage causes remodelling of muscle tissue with hardening (fibrosis) and scarring. The hardened muscle tissue then leads to changes in the conduction system.
Various factors such as enlargement, overstretching and structural can cause these changes of the upper chambers of the heart (atria) and favour the development of atrial fibrillation.
Heart beat off rhythm
Whereas in normal circumstances the so-called sinus node, an area of specialized cells in the right upper chamber, provides a regular rhythm and pulse, hyperactive cells from the left upper chamber take over control in atrial fibrillation. They send out signals in irregular intervals and at times much faster than the sinus node.
Depending on the speed at which the signals are transmitted to the main chambers, the heartbeat is normal, fast or slow. This can turn into a problem if the heartbeatbecomes too fast or too slow and pumping power of the heart or circulation suffer as a result. The irregular sequence of heartbeats is typical for atrial fibrillation.
What increases the risk of atrial fibrillation?
Besides age, there are several factors that provoke atrial fibrillation. Coronary artery disease (calcified coronary arteries), heart attack, heart failure, heart surgery, pulmonary embolism or pneumonia are some major triggers. Since the arrhythmia originates in the left upper chamber (atrium) of the heart and the mitral valve (one of the four heart valves) is directly adjacent to it, any disease or change to this valve can also promote atrial fibrillation.
Also, various drugs such as thyroid medicines, asthma sprays or theophylline occasionally disrupt the rhythm if they are taken in too high doses. Medical doctors speak of a Holiday Heart Syndrome when atrial fibrillation occurs due to heavy alcohol consumption. Larger doses favour this rhythm disturbance.
Sometimes there are situations in which a reason cannot be found. If you have known have atrial fibrillation or if you suffer repeatedly from episodes of prolonged heart racing (tachycardia), we recommend talking to your doctor.
What triggers atrial fibrillation?
In some people, atrial fibrillation occurs unpredictably and seemingly randomly, so they cannot name any triggering situations. In other people with this rhythm disorder, there are typical triggers after which episodes of fibrillation occur.
Hyperactive cells in the upper chamber
In atrial fibrillation, overactive cells from the upper chambers of the heart, the left atrium, fire additional signals towards the main chamber, which can affect the entire rhythm.
In younger people who have not yet reached the age of 50, it often occurs (80%) without any specific heart disease or other medical problem. Doctors speak of "lone atrial fibrillation" or idiopathic atrial fibrillation.
In people over the age of 50, there is often a cause that has led to the arrhythmia. These include, for example, heart and lung diseases or long-term high blood pressure. Let ́s take a close look at the different problems.
Valve disease, poor circulation and heart failure
Between left upper chamber and left main chamber lies the mitral valve. If this valve calcifies, becomes too narrow or no longer closes properly and leaks, it has an indirect effect on the left upper chamber and its cells. This may lead to changes in tension and wall pressure and can promote atrial fibrillation.Coronary heart disease, in which the coronary vessels (coronaries) are calcified and the blood supply to the heart muscle is restricted, can also lead to atrial fibrillation. It also occurs in the context of a cardiac insufficiency and heart failure. The more severe heart failure and shortness of breath are, the more often occurs atrial fibrillation.
Furthermore, atrial fibrillation may occur in the context of heart muscle disease or heart inflammation, as well as after heart surgery. Changes in the electrical conduction system of the heart itself can also trigger the arrhythmia.
High blood pressure, thyroid and lung diseases
In addition to heart disease, there are other circumstances in which atrial cells become overactive. These include longstanding high blood pressure, hyperthyroidism and lung disease.
If high blood pressure is not properly controlled over a long period of time, the heart muscle can thicken and become stiffer and promote the development of atrial fibrillation. An overactive thyroid gland also has this effect. For this reason, doctors always check the thyroid gland's TSH level when new rhythm disturbances occur.
Since pulmonary circulation and heart chambers are directly intertwined, lung diseases such as COPD (chronic obstructive pulmonary disease), severe bronchitis or pneumonia with high fever can also trigger atrial fibrillation.
Alcohol and tablets
In addition to the medical problems mentioned above, excessive alcohol consumption and some drugs can also activate the cells of the left atrium. For example, doctors speak of the "Holiday Heart Syndrome" when people get atrial fibrillation due to drinking a lot of alcohol. This can affect young people on graduation trips and people with an alcohol problem.
Triggers can vary from person to person. Sometimes rich meals, stress or physical exertion can also set off the arrhythmia in people with known atrial fibrillation. Low levels of potassium, a potential side effect of water pills, can also promote atrial fibrillation.
Drugs that may further speed up pulse and rhythm include lung sprays for asthma and COPD. This is because they use similar docking sites lungs and heart. High doses of theophylline, a pulmonary drug, can also generate atrial fibrillation.
Recommendation: Regardless of the reason why you suffer from atrial fibrillation, you may need to take blood-thinning medicines depending on your personal risk of stroke. We always recommend following your doctor’s advice.
Which diseases favour the occurrence of atrial fibrillation?
In addition to age, there are several diseases that promote the development of atrial fibrillation including high blood pressure, heart valve disease, heart muscle weakness (heart failure), coronary heart disease (CHD) and diabetes mellitus.
Overweight and excessive alcohol consumption also increase the risk of atrial fibrillation. All these diseases and factors can damage the vessels and the heart muscle itself, which can affect the heart rhythm. Therefore, early treatment of these basic diseases and the elimination of risk factors are important.
Is stress always a trigger for atrial fibrillation?
Although many patients report that they develop atrial fibrillation especially under stress and psychological strain, stress alone is not always a trigger of atrial fibrillation.
Other people for example experience episodes of atrial fibrillation particularly at rest or at night when sleeping. Activating factors just vary remarkably from person to person. Stress is only one candidate among many.
It is important to find the true source of atrial fibrillation, because once you know what triggers the arrhythmia you can target your treatment. Simply avoiding or minimizing stress does not help in a long term.
Types of AFib
Paroxysmal, persistent and permanent atrial fibrillation
There are three to four different types of atrial fibrillation. The classification into the individual groups depends on how long the arrhythmia lasts and whether it returns to a normal rhythm spontaneously or with the help of medication or electric shock.
Short- and long-lasting palpitations
In fact, the four different types of atrial fibrillation can be distinguished as follows:
- paroxysmal atrial fibrillation
- persistent atrial fibrillation
- prolonged (longstanding) persistent atrial fibrillation
- permanent atrial fibrillation
Paroxysmal atrial fibrillation is a short tachycardia. Within 48 hours, the rhythm changes back to the regular sinus rhythm on its own. Sometimes Episodes may last up to seven days maximum.
Doctors speak of persistent atrial fibrillation if the rhythm disturbance lasts longer than 7 days, but a normal rhythm can be restored with medication or electrical cardioversion (mild shock). They distinguish persistent atrial fibrillation from prolonged persistent atrial fibrillation, which lasts for over a year and is also still treatable.
In persistent atrial fibrillation the rhythm disturbance cannot be converted to a normal rhythm.
Blood thinners
Depending on several risk factors - including age, previous illnesses and previous strokes - you may have to take blood-thinning medication for atrial fibrillation in order to reduce your risk of having a stroke. Doing so, it makes no difference, whether the atrial fibrillation is permanently detectable or only occurs briefly on your ECG.
Furthermore, it is also important that your heart rate is well adjusted and neither too fast nor too slow. If your heart is healthy and beats well, life expectancy is not reduced by the atrial fibrillation itself.
What does AFib with RVR (rapid ventricular response) stand for?
Doctors speak of Afib with RVR when your heart is suffering from atrial fibrillation and beating too fast with a rapid heart rate greater than 100 beats per minute. The ventricles receive only irregular impulses and beat uncoordinated and much too fast - without developing a hundred percent pumping effect.
Risk of heart failure
In the long run, such a fast heartbeat leads to an excessive demand on the heart muscle. The heart muscle may fatigue, and the hearts pump function can suffer. Heart failure with dyspnoea and water retention in legs may result. People with atrial fibrillation with rapid ventricular response do need medical or electrical heart rate slowing therapy.
What is the difference between atrial flutter and atrial fibrillation?
Normally, the heartbeat is determined by the sinus node, a small cell structure in the right upper chamber. In the case of atrial fibrillation, the impulses for the heartbeat are generated from spontaneously firing overactive cells in the left upper chamber. In the case of atrial flutter in contrast, circulating excitations in the right upper chamber lead to the rhythm disturbance. The underlying mechanism is different in these two rhythms problems.
What does "Holiday Heart Syndrome" mean?
The term "Holiday-Heart Syndrome" comes from the fact that high alcohol consumption provokes acute atrial fibrillation.
Atrial fibrillation can occur not only during holidays after alcohol consumption, but also in other situations that are associated with increased stress and strain on the heart muscle. These can include operations, especially on the heart, a heart attack, heart muscle inflammation, chronic lung disease and thyroid disease. Once these diseases have improved, the heart rhythm can return to normal.
Symptoms
What symptoms does atrial fibrillation cause?
Atrial fibrillation does not always cause subjective signs and symptoms. This is also the reason, why many people don't know that their heart rhythm disturbance exists.
Typical symptoms include:
- Heart racing (tachycardia)
- Skipped heartbeat (palpitations)
- Chest pain
- Dyspnoea at rest or on exertion
- Anxiety
- Fatigue
- Lack of resilience
Another presenting symptom can be a new minor or major stroke due to blood clot formation in the left upper heart chamber in the context of atrial fibrillation. If a part of a fresh blood clot is ripped away and flushed into arteries of body or brain.
Can you have atrial fibrillation with slow heart rate?
Doctors talk of slow atrial fibrillation when the left atrium beats fast but only few signals are sent to the main chambers, so that the pulse of the heart is too slow (bradycardia). Sometimes it may not even be able to effectively pump and expel blood.
This rhythm and heart rate disturbance can lead to dizziness, light-headedness and heart failure, but may also not cause any symptoms or discomfort. If no cause is found for the slowed heartbeat in atrial fibrillation (e.g. a heart disease or the intake of certain medications), a pacemaker may be needed.
Which medicines cause a slow heart rate in atrial fibrillation?
Various cardiac drugs can cause atrial fibrillation if the heart rate of the ventricles is too slow (bradycardic).
These can be drugs for heart failure (cardiac glycosides or digitalis), beta blockers for high blood pressure (hypertension) or calcium antagonists for hypertension. If these drugs are responsible, their dose must be reduced or the drugs must be discontinued.
Why can't I feel my upper heart chamber fibrillating?
Atrial fibrillation does not always cause discomfort. Especially when atrial fibrillation occurs only episodically with spontaneous regression, people often do not have any symptoms. The diagnosis is made late or only by chance during a visit to the doctor.
Many people with atrial fibrillation are probably unaware of their condition. People over 60 years of age or with medical conditions such as coronary heart disease, heart failure and high blood pressure should therefore regularly check their own pulse and, if they notice anything unusual, have an ECG checked.
What are typical ECG (electrocardiogram) findings?
In the case of atrial fibrillation, the otherwise regular small waves and larger spikes occur in a disordered manner.
Background
The first electrical stimulus of each heartbeat comes from the so-called sinus node. Its excitation is transmitted to each individual muscle cell of the main heart chambers through further specialized cells.
With atrial fibrillation this process changes. Cells from the left atrium are much more active and generate their own electrical impulses at a much faster pace than the sinus node. However, only a part of these impulses reaches the heart muscle cells; otherwise your heart would beat much too fast.
Complex picture of waves and spikes
The ECG reflects electrical excitation and conduction. The contraction of the main chambers is represented by a large, easily recognizable so-called QRS-complex, the atrial action by a small P-wave, which precedes each QRS-complex in a normal sinus rhythm.
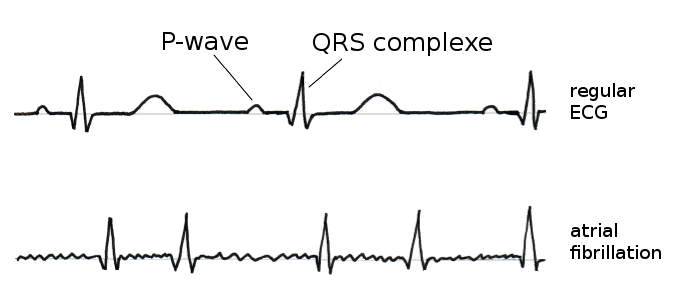
ECG: Irregular and chaotic sequences of P-waves and QRS complexes in atrial fibrillation.
In atrial fibrillation the ECG shows many tiny spikes instead of a regularly occurring P-waves. The ECG baseline appears uneven and QRS-complexes pop up at irregular intervals resulting in a normal, fast or slow heart rate.
The interpretation of an ECG curve is not easy. Only specialists and well-trained personnel can understand the heart curve well. Do not be irritated by computer- analytically pre-printed diagnoses and numerical data on an ECG printout. When a physician evaluates an ECG, history, complaints, medication and many other factors always play a role. We recommend trusting your doctor.
Treatment
How is atrial fibrillation treated?
There are several ways to treat atrial fibrillation. Physicians distinguish between rate and rhythm control. Treatment of atrial fibrillation itself is not so simple. Some drugs like betablockers can slow down a fast heart rate, to ensure that the resting pulse does not exceed 100 beats per minute.
For more severe symptoms and frequent episodes of atrial fibrillation, so-called antiarrhythmic can help. They counteract the rhythm disturbances and are supposed to keep the rhythm stable. However, in the long term, these do not always work reliably and are not free of side effects.
Furthermore, procedures like electrical cardioversion, catheter ablation or even surgical interventions help to re-establish sinus rhythms.
Pills in the pocket
In addition, there are so-called medications on demand that interrupt an attack of atrial fibrillation. This "pill in the pocket" concept is particularly beneficial to otherwisehealthy people. It stops heart racing attacks due to atrial fibrillation within only few minutes.
Watch out for signs of heart racing and palpitations
In order to be able to treat atrial fibrillation at all and protect against a stroke, it must first be detected. And this is not so easy because the symptoms are often very unspecific.
If you notice an irregular heartbeat every now and then or even a racing heart, you should pay attention. Have this checked by a doctor for safety reasons. If you have a well-founded suspicion, he will then arrange for an ECG. Since atrial fibrillation can occur in attacks, it is often necessary to carry the ECG device with you for 24 hours.
Can atrial fibrillation be permanently eliminated with medication?
In most cases, atrial fibrillation cannot be permanently suppressed even by taking medication. However, sometimes simply lowering the heart rate without eliminating the atrial fibrillation is enough (frequency control).
Independently from rate and rhythm control, blood-thinning medications are used to protect patients from blood clots, embolism and stroke. Often blood thinners have to e continued, even if doctors were able to restore your heart rhythm.
Cardioversion
What is more effective - drug or electrical cardioversion?
Electric cardioversion is considered by many experts to be the a very effective way to restore a normal heart rhythm in patients with atrial fibrillation.
Young patients and people with new onset of atrial fibrillation
Electrical cardioversion is often successful in younger people with new or „newish“ onset of atrial fibrillation, or who suffer from cardiac discomfort like chest pain, light headiness or shortness of breath.
However, not everyone will benefit from electric cardioversion, and it should only be attempted if there is a good chance of success. Whereas in the past, electrical cardioversion was performed faster and more frequently, today we see this in a more differentiated way.
How successful is electric cardioversion?
Immediately after electrical cardioversion, the success rate is about 90%, a large proportion of patients goes back to normal sinus rhythm. However, some people relapse hours or days after cardioversion. Sometimes certain cardiac medicines can help to keep more people in sinus rhythm.
Elderly people with long lasting atrial fibrillation on the other hand to relapse more often. Structural changes especially in the left upper chamber restrain a successful cardioversion and frequently go along with relapse. Plus, clinical studies have shown, that rate control is not inferior to rhythm control (cardioversion) in terms of disease and death frequency in these patients.
Can electrical cardioversion be repeated several times?
Yes, electrical cardioversion can theoretically be repeated several times. There is no fixed upper limit as to frequency and repetitions. Yet, every cardioversion is also associated with risks, which somewhat limits the possibility of repetitive treatment trials.
In addition, relapsed atrial fibrillation after electrical cardioversion is an indicator that cardioversion alone may not be enough. It increases the probability that after a second or third cardioversion, the heart rhythm will not be permanently restored. Success rates may be increased with antiarrhythmic drugs.
Catheter Ablation
What is the role of the pulmonary veins in atrial fibrillation?
Atrial fibrillation often generates from overactive cells right around one or more of the four pulmonary veins in the left upper chamber, where blood, rich in oxygen, exits the lungs and enters the heart circuit. This is where catheter ablation comes into play. By using high frequency electricity or heat overactive areas in this region can be destroyed. In certain patients this procedure can stop atrial fibrillation.
Can atrial fibrillation be treated with catheter therapy?
Yes, atrial fibrillation can often be treated with catheter ablation. This alternative is particularly useful if the drug treatment does not lead to a satisfactory reduction of symptoms.
With catheter ablation, starting points of the left upper chamber that cause atrial fibrillation are sclerosed and thus immobilized. So, the faulty electrical impulses can no longer be generated. Thus, the heart action can be permanently restored to normal.
Despite great success rates of catheter ablation in atrial fibrillation, this procedure cannot be performed in every patient. There certain requirements that must be fulfilled. Also, sometimes atrial fibrillation may re-occur making a repeat procedure necessary.
When can the success of a catheter ablation in Afib be re-assessed?
The success of catheter ablation in atrial fibrillation is not always immediate and can often only be assessed months after the procedure. Episodes of atrial fibrillation may still occur in the first few weeks without a reliable statement about the success of the treatment.
If the atrial fibrillation has not improved after several months, the procedure can be repeated after three to six months. Repeated ablations (i.e. sclerotherapy by catheter ablation) are not uncommon. Sometimes only subsequent ablations bring the resounding success.
Atrial fibrillation: New Therapies
There are signs of progress in the treatment of atrial fibrillation. Several new drug approaches to treat cardiac arrhythmia are currently being tested.
Angiotensin receptor blockers against atrial fibrillation
Beside heart rate slowing drugs as betablockers or digoxin there are other antihypertensive drugs that have positive effects on atrial fibrillation. So-called Angiotensin receptor blockers belong to this group. Angiotensin receptor blockers inhibit the body's own hormone angiotensin (hence the term angiotensin II receptor blocker) and a reduction in angiotensin not only reduces blood pressure but also the tendency of scarring in the atrial tissue. This may prevent and reduce episode of atrial fibrillation.
Yoga stabilizes heart rhythm
Also, yoga may help against atrial fibrillation. An US study showed that the heart rhythm disorder could at least be slightly reduced with regular yoga exercises.
In the study, 49 patients with atrial fibrillation were included in a three-month yoga training session in addition to usual therapy. They were compared to a patient group that was able to pursue a sporting activity of their choice.
Fewer episodes of AFib with yoga
Even with the yoga exercises, only a small proportion of patients experienced a reduction in the time of atrial fibrillation (3.8%). Compared to non-yoga patients, however, this was an improvement of about 50%. According to the authors, yoga has a calming effect on the heart rhythm through its meditative effects. Even if the study results were not impressive, one can at least imagine that there is something to it.
Why does atrial fibrillation often worsen over time?
Atrial fibrillation itself leads to further changes in the heart muscle cells in the area of the atria that maintain the process of fibrillation. Because of changes in cell metabolism and cell membrane those cells are more easily activated electrically. This maintains the process of circular heart excitation or arrhythmia. Sometimes a form of vicious circle can develop, and atrial fibrillation can occur more frequently and for a longer period.
Does temporary atrial fibrillation (AFib) always develop into chronic AFib?
Whether a one-time event of atrial fibrillation or episodically occurring atrial fibrillation turns into a chronic rhythm disorder cannot be determined easily in advance.
Sometimes atrial fibrillation disappears completely, for example after the treatment of underlying diseases. In addition, treatment often succeeds in normalising the heart rhythm in the long term. The earlier the treatment begins, the better the prognosis for a successful therapy. If, on the other hand, atrial fibrillation persists for longer, it is not always possible to normalise the rhythm.
In the long term, however, atrial fibrillation often develops into a chronic disease.
Should I retire because of recurrent atrial fibrillation?
Heart rhythm disturbances caused by stress and strain at work are perceived as threatening by many of those affected. Depending on the severity of symptoms and a possible consideration may be to retire. However, it also plays a role which country you live in.
But even without stress at work, situations are likely to occur that make the heart skip a beat. For this reason, adequate treatment of atrial fibrillation is very important to prevent repeated attacks of atrial fibrillation in stressful situations. The treatment focus should therefor lie on eliminating not only stress but also the underlying causes the cardiac arrhythmia.
Complications
What are risks associated with atrial fibrillation?
An irregular fast beating heart can have difficulties pumping effectively. Its ejection fraction may decline. Dyspnoea and at time chest discomfort may be first signs.
Atrial fibrillation may furthermore lead to a reduced blood flow in the left upper chamber, which increases the risk of blood clot formation and is associated with an increased risk of stroke.
Another complication of atrial fibrillation consists in a weaker heart muscle that may no longer be pumping properly. This can lead to a worsening of the disease, especially in cases of already existing heart failures (cardiac insufficiency).
Problem stroke
Some people with atrial fibrillation are at increased risk of having a stroke. Because of the irregular heartbeat, blood may flow more slowly in the left atrium or the atrial ear, a small bulge, so that a blood clot may form. A small piece of such a clot can break off, travel through the main chamber of the heart, the artery and the neck vessels into the head and close a vessel there. A stroke can follow.
To prevent such complications, doctors prescribe blood-thinning medication. Who benefits from such substances depends on the overall risk. Factors such as age and accompanying illnesses play a role.
Problem rapid heart rate
A second problem with atrial fibrillation occurs when the heart beats too fast or too slow. If your pulse exceeds 150 beats per minute for several days, your heart can get tired in the long run. The pumping force decreases, possibly resulting in cardiac insufficiency, which causes water to back up into the pulmonary circulation or even into the abdomen and legs.
Medications such as beta blockers help to regulate the pulse. In certain situations, doctors can use electric cardioversion to bring the heart back into a normal rhythm. Over the course of weeks and months, however, it is not uncommon for atrial fibrillation to break out again.
In selected individuals, electrophysiological examination and ablation may be able to stabilize the rhythm in the long term. However, this examination is invasive (like surgery) and cannot be performed in all people with atrial fibrillation.
Does atrial fibrillation increase the risk of stroke?
Yes, although the risk of stroke in younger people with atrial fibrillation is significantly lower than that of older people. People under 65 years of age who are healthy except for their atrial fibrillation have a risk of less than 1% of suffering a stroke within the following year. The risk rises to over 6% in people over age 65 with additional heart disease. Whether or not a stroke occurs also depends on concomitant diseases such as heart disease.
A study has now shown that the prevention of strokes in atrial fibrillation is not always optimal. According to the analysis, only every second patient with cardiac arrhythmia receives adequate stroke protection, especially in smaller hospitals and general practitioners' practices. Such protection mainly consists of blood-thinning therapy. A permanent intake of anticoagulant medication necessary.
Blood thinners and anticoagulants
To prevent blood clots from forming or clotting during atrial fibrillation, patients are given blood-thinning medication, also known as anticoagulants. Blood thinning is important because blood clots can be flushed into the bloodstream and cause life-threatening vascular occlusions (embolisms).
When do I have to take anticoagulants?
The following five factors increase the risk of blood clot formation and stroke in people with atrial fibrillation:
- Reduced heart pumping ability (cardiac insufficiency, heart failure)
- Previous embolisms
- High blood pressure (hypertension)
- Age over 75 years
- Diabetes mellitus
People with one or more of these risk factors should take blood thinning medication. Taking blood thinners prevents the formation of blood clots.
New oral anticoagulants
A new group of drugs seems to make it easier to prevent strokes in patients with atrial fibrillation. Experts from the German Society of Neurology have now pointed this out.
The most known blood thinners are so called vitamin K antagonists as warfarin and coumadin. They have been on the market for many years. One of the disadvantages is, that blood tests are unavoidable in order to control adequate dosing.
In the decades a few new drugs have entered the market, they are called new oral anticoagulants (NOACs). Depending on the product, some of them have shown to reduce the risk of stroke as effectively as the old drugs, but with fewer bleeding complications.
What is the CHADS2 score?
The so-called CHADS2 score is used to estimate the risk of stroke in patients with atrial fibrillation.
The capital letters stand for:
- C = Congestive heart failure
- H = Hypertension (high blood pressure)
- A = Age
- D = Diabetes mellitus (diabetes)
- S2 = previous stroke or circulatory disorder in the brain
Up to six points are distributed, whereby the risk increases with the number of points. The value is of practical relevance, e.g. regarding the choice of a blood-thinning therapy.
Short facts to INR and Aspirin
Taking blood thinners like warfarin or coumadin intends to prevent blood clot formation and stroke. The target value in these cases is an INR of 2.0-3.0.
Life expectancy
Can I die from atrial fibrillation?
Usually, people do not die directly from atrial fibrillation. However, the consequences of fibrillation can be life-threatening such as blood clot formation. It is particularly dangerous if an artery that supplies blood to the brain is blocked, because this can lead to a stroke. The danger of a stroke depends on which area of the brain is affected and how much brain tissue is destroyed.
Does atrial fibrillation reduce my life expectancy?
Atrial fibrillation does not necessarily reduce life expectancy if the arrhythmia is treated. Especially people under 65 years of age without further heart disease are not expected to have a reduced life expectancy due to atrial fibrillation.
Also, older people and patients with additional heart disease benefit from modern treatments, so that they have a significantly higher life expectancy than in the past.
Normal life expectancy
Atrial fibrillation is one of the most common cardiac arrhythmias. The probability of this increases with age and with certain risk factors such as high blood pressure, heart disease or alcohol consumption.
Atrial fibrillation will not shorten your life expectancy while your pulse is well adjusted, you are taking blood-thinners when necessary and indicated and you do not suffer from severe heart failure.
For the prognosis, however, it is very important to identify and treat underlying and perhaps previously unknown heart diseases such as coronary heart disease. In order to generally keep life expectancy as high as possible, all accompanying diseases must of course be treated.
Life expectancy independent of treatment
The type of treatment itself does not change your life expectancy. Whether your heart is stabilized with beta-blockers, where the fibrillation itself usually remains, but the pulse is slowed down, or whether a normal rhythm is restored with cardioversion or ablation procedures makes no difference. Rate and rhythm control are equally good.
An exception are patients with severe heart failure in addition to atrial fibrillation. They may benefit from achieving and maintaining a normal rhythm (sinus rhythm) electrically or with medication.
Authors: Susanne Endres MD, Julia Hofmann MD & Jörg Zorn MD
Sources:
- ESC Clinical Practice Guidelines 2016: Atrial Fibrillation (Management of) Guidelines
- Competence Network Atrial Fibrillation